Nia’s Neo-natal Intensive Care Unit (NICU) Journey is the most difficult thing I/We’ve ever experienced, which is why it’s taken months to write.
In honor of NICU Awareness month, I share our story.
It was a blessing yet unfathomable, unrelenting, traumatic, joyful, dreadful, overwhelming, awful (at times), and a roller coaster ride- full of ups and downs. September 27, 2017, December 5, 2017, and January 24, 2018 are three dates I will never forget!
Spending 118 days in the NICU- two different hospitals might I add, was nothing we ever expected… but let’s be honest we weren’t expected to have any days beyond Nia’s birthday with her- so for that we are thankful.
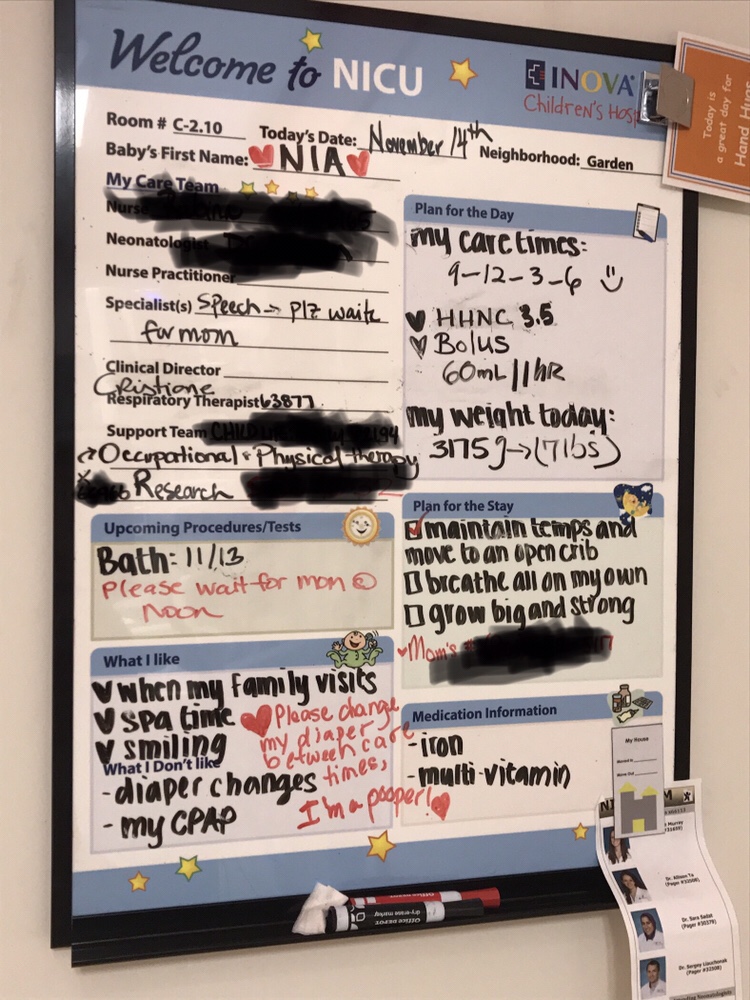
I can’t ever get the smell of the hospital out of my nostrils- the monitors, the alarms- various beeping sounds, smell of Poly-vi-Sol, Palmolive dish detergent, cords everywhere, and my dry skin from scrubbing in and out of the NICU God knows how many times a day! Care time- was also unforgettable- a gift and a curse (more on that later).
There were many “firsts,” but the biggest one yet was holding Nia for the first time- over 55 hours after giving birth! The wait felt like an eternity, BUT It was an incredible moment. I cried tears of joy- completely in awe of God’s miraculous work! Then Nia’s first sponge bath, approximately a week later- she graduated to a big girl crib and her first non-hospital sponsored (required) baby outfit!
First Time Holding Nia- 55 hours after giving birth- September 29, 2017


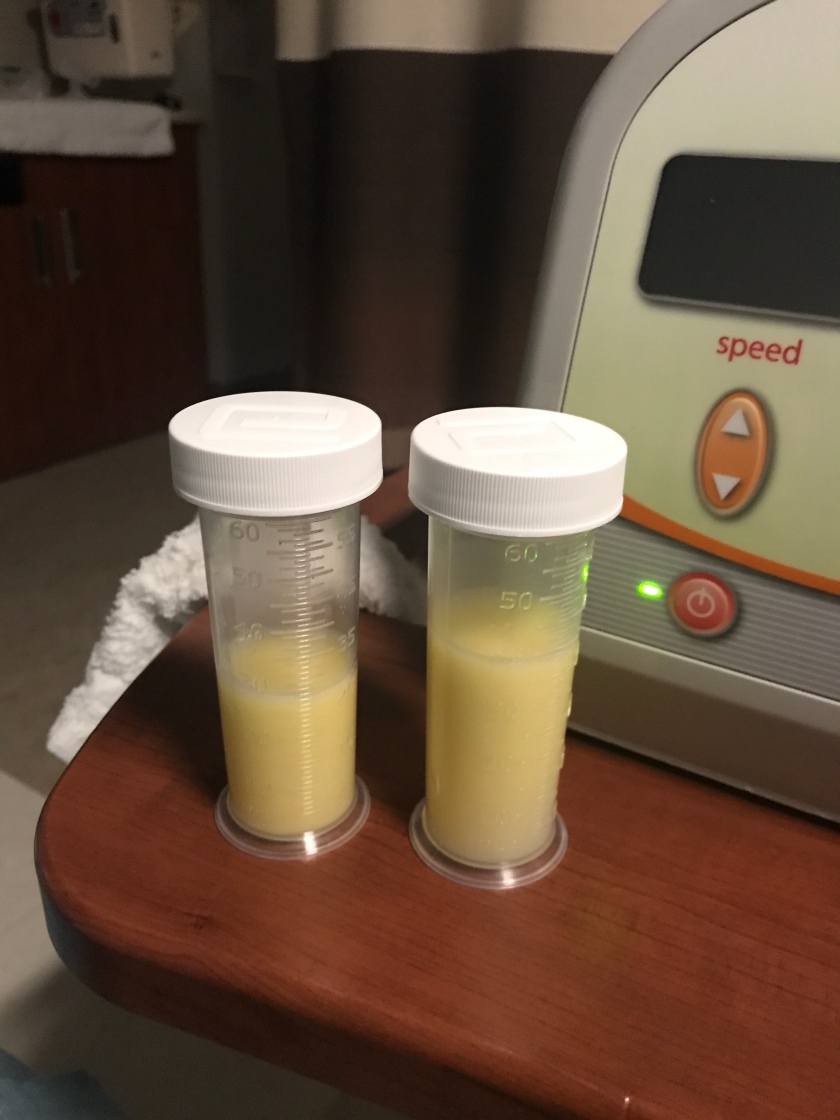
Exclusively Pumping Mama
Beyond firsts for Nia was a huge first for me- adjustment to pumping life! As a NICU mama warrior, I committed to providing Nia all the breast milk my body would produce for her- thank God I had a great supply despite exclusively pumping (EP). For NICU mamas it is hard seeing your baby endure and the only thing you may have control over is pumping (if you choose or are able to do so)- feeling like a cow 😂 and more pumping to give your baby the best medicine possible! However, Being an EP mama did not come without a sacrifice and at times overwhelming because it took precious time from Nia and a race against the clock for her next care time (diaper change, temperature check and ever 12 hours changing the CPAP from mask to bonnet), despite being able to pump in her private room. For breastfeeding mamas it’s already exhausting, but just imagine being attached to a machine for 6-7 times a day, while trying to manage medical team members stopping in (sometimes) while you are pumping and taking in information about your baby’s care. However, I refused to quit (AND STILL GOING STRONG)! At times pumping was a good distraction from our reality and sometimes chaotic life that was centered on essentially living in a hospital.
The Beginning of a Long, SLOW Journey
Since Nia came out pink and screaming, and requiring non-invasive respiratory support, Antoine and I thought we might spend a month in the NICU at best (ridiculous thinking, so naive I guess), not 118 days- 2 days shy of 4 months.
The First Day/Night- Rewind
Before I ever held Nia, I will never forget my first time seeing her in the NICU. I worked to get myself together quickly despite having a C-section that morning! I made my way to her NICU neighborhood- the Garden and scrubbed in. I will never forget being wheeled to Nia’s room and being able to stand solid on my two feet straight up- with no regard for my fresh incision just to witness, see and touch my/our living miracle. She was perfect- all 12 Fingers and 10 toes! She was breathing with non-invasive respiratory support and a little oxygen- CPAP pressure of 6 and oxygen at 23 percent (room air is 21 percent)!
Antoine became an immediate super dad! He literally would take the small syringes and eventually “snappies” bottles provided and ensure the little colostrum aka liquid gold I produced was expedited to Nia! He ran downstairs to the NICU after each pumping session and washed all my pumping parts! I didn’t have to lift a finger- a complete blessing!
The beginning of liquid gold in NICU “snappies”
Fast forward to my discharge day!
My heart sank at the thought of leaving Nia alone for even a short amount of time! I didn’t officially discharge until closer to 7pm because it was unfathomable to leave our baby. Initially, she had great nurses, but a core team would’ve been preferred. However, that didn’t always come easy!
Antoine taking a peak at his precious miracle- oh the joy (see the soft smile on his face)- PROUD DADDY!

Antoine first time holding Nia!!!

Leaving the hospital! We were so excited to be new parents but sad to leave Nia.Our Baby Girl was breathing- nothing but the blood of Jesus!!!! Antoine’s Shirt Credit- gift from his faternity- linebrothers

The First Full Week
Within the first week of Nia’s NICU stay we began to understand the routine of things. Rounds by the neonatologists (NICU doctors) were from 9am-11am. Monday rounds seemed to always be the biggest since it was the beginning of the week- changes to feeds, respiratory support would likely happen. The weekly labs sucked for Nia because she was a hard stick- meaning her blood either hemolyzed too fast or they couldn’t draw enough. Initially she had weekly x-rays to ensure her naso-gastric (NG) feeding tube was placed in the right location. Nia also had routine echocardiograms to ensure her Patent Ductus Arteriosus (PDA) closed; to ensure her atrial septal defect (ASD) remained stable; and to double check for ventricular septal defect (VSD). The cardiology team watched closely for that because it would be something else to complicate her heart defect. Thank God the PDA closed on its own and no signs of VSD, which would’ve definitely put Nia in the operating room before 6 months old.
Crib Life

Driving the Train for Nia- Month 1
The first 2 weeks Antoine and I spent about 8-9 hours during the day. We would leave and come back for a few hours at night. When Antoine returned to work, he would go in really early so that we could have most of the afternoon and night with Nia. After 30 plus days NICU fatigue set in! If you’ve had an extended NICU stay you know what I mean!
NICU Parent Warriors- Advocates!
As NICU parents it is critical to advocate for your baby/babies and convey that you understand how things operate and you are educated on your baby’s condition, and ask questions. We learned Nia had to initially have a peripherally inserted central catheter (PICC) line because she needed additional nutrition- TPN. That meant we couldn’t see her for at least 12 hours because the environment had to be sterile. Thankfully, the PICC line didn’t stay too long.
Nia had two attending neonatologists that rotated weekly between one another. One of her neonatologists had exceptional bedside manner, open-minded and willing to explain his thought process. When we felt like we were on a good foot, the rotation would change, and at times led to mis-communication. In this learning process, we also understood early on that family meetings are useless unless the medical specialists (i.e. cardiologist, pulmonologist) are part of the conversation.
A sense of frustration grew because there was no clear direction of what to expect as it related to Nia’s care plan. I discussed with the medical team that Nia’s rapid breathing couldn’t be addressed the same as a preemie baby because her lungs would always be smaller- because of Ellis-van Creveld (EVC) complexities! That seemed to fall on deaf ears and we received the response that the medical team had treated rapid breathing over and over again and how they were treating her lung condition was a normal course of action!
Caveat: INOVA Fairfax is outstanding for preemie and micro-preemie care as a NICU Level IV institution, but Nia did NOT fall into those categories. This NICU only had seen one other EVC case in five years prior to Nia’s birth, because her condition is so rare- 1 in 60,000 births and less than 300 cases reported globally.
By the end of month one Nia appeared ready to wean from CPAP to a high flow nasal cannula (HHNC), which came two days after she turned 1 month! Things seemed to be going well, but there was no real discussion of discharged plan. The biggest thing pushed on us was nutrition and slower breathing, so I continued pumping but never stopped wondering how to get Nia out the NICU. In the back of mind was the hospital I had found doing research while I was still pregnant…
In the midst of Nia making overall good progress, her bottom (butt) had a complete breakdown- beyond a normal diaper rash. That’s when I turned from diplomatic Erica, to Mama Bear. Why is her butt broken down???? I had been at the NICU 9-10 hours a day, what were the nurses doing- forget care time! Nia was quite the pooper in the NICU, and I had to literally spell out to some of the nurses (UGH) why her diapers had to be changed before care time. If Nia poops 30 minutes after her initial care time, she can’t be expected to sit in it for the 3-4 hours- RIDICULOUS and not acceptable. This was not my first discussion about this- I was over it- and expressed my frustration to both nurse managers! In return her board was updated- I’m a pooper.
Nia was a good and overall stable baby in the NICU, but at times that assessment also came with a cost. We were thankful she was less critical than some of the other precious babies, however she would at times seemed to be ignored or not checked until care time by the nurses. So I made a point to start spending 14- 16 hours a day. I know a lot of people thought well at least your baby is being cared for and you can get some rest- just because my baby is not home doesn’t mean I am resting well! I would rather have sleep deprivation because Nia was at HOME.
In between trying to care for Nia there were other logistical things we had to think about- getting food everyday, checking on our home, making sure bills still got paid, oh and making sure our fur baby– Miles was cared for! Antoine handled most of these things and we had amazing friends and some family that made sure we had food from near and far!
A Little Fun in NICU Life
There were some happy and fun moments in the NICU… Nia would have fun onesies that cracked everyone up… We had to laugh to keep from crying some days!
Nia- The Pooper- Diaper Loading Please Wait! 😆

Halloween 2017- Dr. Nia! Halloween Sign Credit- NICU Nurse

Sign Credit: Sweet NICU Nurse
Back to Discussion with doctors…Advocating for Nia
After so many questions and no straight answers, I remembered from some research that I had conducted while pregnant- learning and getting up to speed on EVC- there was one particular children’s hospital that specialized in treating dwarfism and more specifically EVC- Nemours/AI duPont Children’s Hospital in Wilmington, DE. This hospital is about two hours from the DC area. I asked Nia’s favorite neonatologist would he be amenable to a conference call with the medical team there so we can gain a better sense of Nia’s care plan as a baby that has EVC. He was open to it!! He always wanted the best for Nia- despite being a LSU grad- LOL! (We talked SEC football non-sense since Antoine and I are Ole Miss alum).
Month 2
INOVA Fairfax Medical Team Conference Call With duPont
Thanks to our awesome genetic counselor at Fairfax, she was able to coordinate the conference call with duPont and Nia’s favorite neonatologist. We were not on the call but our genetic counselor took lots of notes. We learned that Nia’s oxygen saturation parameters should be different than other babies because of her heart defect- ASD. That was a blessing as Nia was still being treated similar to a “textbook” case preemie baby/ which she never was. I tried to articulate this message over and over! We learned there were some amazing doctors part of this duPont EVC team- from neonatologist, pulmonologist to cardiologist- All this would be important later…
Nia Turned 2 months andddd Stopped Breathing- Advocacy Became Critical
At 2 months, November 27, 2017- less than a week after Thanksgiving, Nia overall looked great- though still breathing pretty rapidly. She was now down to oxygen only – no CPAP at just around .4 liters of 100 percent oxygen. The weekend leading up to turning two months- Antoine and I noticed her chest retractions were more defined than usual and she was a little congested and seemed more tired than normal. We didn’t think much of it initially. Antoine seemed a little stuffy as well, but nothing more and decided he would wear a mask as a precaution. Well the mask led to him being asked several questions by the medical team- are you sick? The problem with the questioning was there were medical team members walking around coughing, and sneezing with no masks/ but no questions asked of them- since I am assuming they “didn’t need to a mask”- whatever!
I digress, well for the first time while Antoine and I were at the hospital together, we decided to go off campus for lunch. We were completely burnt out on Panera inside the hospital. It’s a nice option, but two months straight of Panera whew! Upon our return to the NICU from lunch and walking into Nia’s room, we were met by her attending resident. She let us know that Nia had to be bagged- what!!! She immediately said everything seemed okay, Nia was just working harder to breathe so they moved her from low flow oxygen back to high flow pressure and oxygen to decrease the amount of work she was having to do. Okay…
Fast forward… Antoine stepped out to get something to drink while I finished pumping. I was finally ready to pick Nia up with the assistance of our favorite NICU nurse (now forever friend), and Nia’s O2 saturation levels started to dip below her normal parameters for her ASD heart condition, and then her lips turned BLUE, and my baby looked back at me for the first time with fear and panic in her tiny eyes! The nurse looked at me and said I am so sorry but I have to call a MSET. I knew we were in bad shape before that call but it literally seemed like pandemonium had happened. Doctors and nurses were running from everywhere. Nia had to be bagged over and over again!!! Being in the NICU for 60 days at this point I had seen this MSET call before just not for my baby 😭…I literally fell apart- inconsolable tears and a couple of nurses comforted me. Lord did you bring us this far to take our baby from us! I couldn’t wrap my heart and mind around what was happening. I went out to the Parent Lounge to let Antoine know what had happened.
At this point the doctors were thinking virus or bacterial infection. so a lot of tests were ran.
Nia’s favorite attending neonatologist- finally came to the parent lounge and he didn’t have a warm look. His face looked very serious and concerned. Antoine and I thought is this doctor coming to tell us Nia had died… I just couldn’t fathom how things had changed in an instant.
He informed us she Nia finally somewhat stable, but her breathing was incredibly fast. She was on the verge of intubation- say what! Nia had never been intubated before despite her condition, and that apparently is rare. He said they would have to keep watching her and if she continued to work any harder to breathe, intubation was still on the table- which he really didn’t want to do! He truly believed in Nia.
He informed us that they were running tests because he believed she had caught a cold from Antoine. Of course all types of anger and guilt set in. First thought was, we were cautious, second thought we were offended- one of these nurses could’ve given her a cold.
That night Nia sucked on her paci so hard that she made one of her natal teeth bleed and it had to be pulled with tweezers.
In the midst of the chaos, tests slowly started to come back and they showed no sign of infection.
I planned to return to work the next day, but clearly God had other plans. I set a schedule to work 40 hours every two weeks and 40 hours of Family Medical Leave Act (FMLA) leave without Pay (LWOP), so I wouldn’t tank all of my leave prior to Nia coming home. Instead another week of FMLA LWOP- the cons of federal employment….no true maternity leave.
Before we stepped out to lunch! Nia’s 2 month photo- before the day turned south
After the second time Nia stopped breathing!! Back to CPAP (which was set at 7- higher than when she was born) while praying for no intubation

Fast forward, the next day…Nia was doing better, and all tests were negative for infection. In the midst of this I made a call to the EVC cardiology expert that had been on the duPont conference call. She knew exactly what had happened to Nia. Nia likely had an hyper-cyanotic episode- hence turning blue. These episodes can happen in EVC babies with no clear cut explanation. Over oxygenating EVC babies can cause similar responses, which we learned later was mostly likely the case. The cardiologist informed us she or the EVC team couldnt treat Nia so far away and we need to transfer her ASAP.
We decided to do just that. I informed Nia’s favorite neonatologist that it’s best we do so. I also had a candid discussion with him that we were offended that he initially concluded that Antoine made Nia sick. He apologized and said he initially believed Antoine had gotten Nia sick. Nonetheless, the neonatologist supported the transfer and genuinely wanted the best for Nia (He continued to check on her)!
Prep to Transfer- First visit/meeting to duPont
This process was fast! DuPont contacted us on Friday, and we set up an appointment to travel to Wilmington, DE on Monday to meet with the medical team there to see if this would be the place for Nia’s care. We met with the Cardiac team, Chief of Pulmonology, and Chief of Neonatology along with the neonatal nurse practitioners (NNP)that were part of the EVC expert care team. They showed us a FLOW CHART of how the intake process works for EVC babies- WOW!!!!! We were impressed! Nia would have a G-tube placed within a few days of arriving to DuPont.
We had been waiting for a while for this surgery to happen at Fairfax, but there had been a conservative approach to do so (Nia was actually scheduled for this surgery prior to her coding), while at DuPont it was probably one of the first surgeries that many EVC babies have and within two weeks of birth. Nia was already 2 months old! Now keep in mind duPont’s NICU aesthetics was not nearly as nice as Fairfax but as long as she could get excellent care- it didn’t matter!!! While we were on our visit, the social worker informed us we had been approved for transfer, and that we needed to move on it ASAP! Antoine thought we would have at least til Wednesday, and the answer was NO- NOW- tomorrow!!!!
At that moment- I can’t lie, anxiety set in- the reality of what would be the cost to transfer Nia, how would we manage our home, the cost of traveling back and forth from the DC area to Wilmington and all the toll fees especially with me not working full time at this point. Then there was God, reminding me how he has never failed us yet- He has brought us this far to even be at this point with Nia! It will work out! I am forever reminded- of Phil 4:19- But my God shall supply all your needs according to His riches in glory by Christ Jesus.
Word spread fast back at Fairfax that we were planning to transfer Nia. Apparently there was rumint of it over the weekend, but the fact the process was expedited was even more shocking. I had just met with the Clinical Director over the weekend to demand a formal Care team- but that point was null and void….Nia time was up at this NICU and we were ready, yet it was so bittersweet.
Medical Transfer/Transport Day- Road to Dupont- Wilmington, DE
December 5, 2017– Transfer Day was filled with many emotions as this NICU had become our second home. A lot of the staff couldn’t believe we were leaving. The medical team expressed how gracious I had been as a NICU mom, yet advocating for Nia to no end! We definitely had nurses and some families we would miss and a couple of the doctors, BUT we did not regret transferring Nia. She deserved a team that knew how to care for her complex condition.
The transfer was seamless! Dupont’s medical team arrived via their own ambulance and transport incubator. Nia was pissed and not happy to be put in this enclosed case. So many people came by to see us off! Nia truly had won and touched the hearts of so many people in just two short months, despite some of the frustrations we faced in this NICU.
Transport Day- Portable Incubator that Nia hated! 
The team loaded her up and we made our way to the ambulance. I was able to ride in the transport with Nia while Antoine drove separately and met us there! Two hours from home here we go…
Nia’s Arrival to Nemours/A.I. Dupont Children’s Hospital
Nia arrived at Dupont Children’s Hospital and immediately became unhappy again when the ambulance stopped moving! The transport team made their way with Nia to the NICU and we had to wait in the parent lounge until she was all checked in. They had her on pre-cautionary contact isolation for MRSA just because she was a transfer. Finally, the charge nurse came and got us, she was also Nia’s nurse until night shift. I must say we loved Nia’s night nurse (she signed up to care for Nia every night she worked!

We knew it was an older NICU from our first initial visit, although other parts of the hospital were new. The first thing we noticed was this NICU was much smaller than Fairfax. There wasn’t a 21st century feel to the rooms, and some rooms were doubles not single. At Fairfax, every baby had their own private room for the most part, unless you were a twin.
For the time being Nia had her own room, but we were immediately informed this could change once the team felt she was stable. We were advised that specialists would be by to speak with us the very next day- whoa this place was fast. We had planned to leave Nia and come back on Thursday- which I believe God knew I wasn’t prepared for the separation. However, we had no clothes or anything for an overnight stay.
We requested to stay at the Ronald McDonald House of Delaware, but they were full! So we had to stay at the hospital overnight, but luckily Ronald McDonald had a couple of overnight rooms at DuPont where we could at least shower and one parent could sleep- Antoine took the room and I stayed with Nia. We went on a Target run before midnight to get a few necessities- changing clothes and toiletries. By that morning we were contacted by the Ronald McDonald House we had a room available! Thank God! That really helped to cut the expenses for lodging.
That same morning the pediatric surgeon met with us to discuss Nia’s G-Tube and Fundoplication (Nissen) surgery. A nissen is when a little portion of the stomach is wrapped around the esophagus to prevent aspiration, which could be deadly for Nia if it got into her lungs. He is specifically the expert for EVC babies g-tube surgery because he understands their unique anatomy. He explained to us what to expect, including how long the procedure would take- approximately 45 mins or so, and how quickly Nia would start feeds via her new feeding tube, which was no later than the next morning. We were shocked because at Fairfax their approach was a little more conservative- somewhere around the 3 days or more mark would be the slow introduction of feeds. Nia’s surgery was quickly scheduled for Friday, December 9, 2017- only 3 days after her arrival at DuPont.
Later that morning all the other specialists came to met with us- the chief of the cardiac ICU and the chief of pulmonology. Nia would have another echocardigram to ensure her heart defect remained stable as it appeared from previous visuals. The pulmonologist discussed the condition of her lungs and current respiratory support. It was indeed a long day but well worth it because these doctors definitely worked together as a true interdiscplinary team. They had weekly discussions and rounds of complex medical cases. Our hearts and minds were finally at ease. We felt okay to leave Nia for a day or so.
We drove back home to the DC area (Alexandria) that night. I cried leaving Nia, not because I was worried about her care, but being two hours away meant I couldn’t just hop in my car like at Fairfax and be at her beside in 25 minutes. It would be only the second time we hadn’t seen Nia in a 24 hour period since she had been in a NICU. We quickly returned in the wee hours of Friday morning so that we would be at Nia’s bedside prior to her G-Tube surgery.
G-Tube Surgery Day
We arrived at the hospital around 7:30am as they had planned to take Nia for surgery by 8:30am. When we arrived she was unclothed outside of her diaper and a white hat. She was awake as if she had been waiting for us to come back. Around 8am the cardio-thoracic anesthesiologist came by to explain his role- which we were surprised about that! That’s pretty awesome- totally unexpected and had not been a discussion before, but again DuPont understands the complexity of EVC babies. The surgeon quickly stopped by and then the surgery team arrived to take Nia away. I shed tears for sure- and we prayed over her. Out the room she went- but not before a couple last minute pics. We felt at peace but for any parents it’s still nerve wrecking for your baby to be taken away even if it is a “simple” procedure. Any procedure for Nia is never simple.
Last pic before doctors took Nia for her first surgery

Nia came back from surgery intubated, which was a little scary. She was awake but initially couldn’t make any noises then we started to hear her little cry despite her being intubated- that was a little hard to hear. The respiratory therapist thought Nia would stay intubated for possibly 24 hours. However, the attending neonatologist and NNP disagreed. They believed in Nia and overrode the RT and said “nope we are pulling it.” Nia’s O2 saturation initially started bottoming out, but the team didn’t flinch. They were so calm and got Nia respiratory support under control- she was extubated within 2 hours of surgery, which was a huge shock! 🙌🏾🙌🏾
Nia was in pain the first 24 hours but after that she did well! On Sunday, we left Nia to go back to the DC area for work for a couple of days. That was incredibly hard to do.
Two days post surgery 
For the next three days I finalized the logistics for living and working in Wilmington. I left Antoine back in DC and headed to be with Nia. It was hard leaving Antoine because we are a team and He has been on this journey with me- but Nia needed me by her side. It felt so good to have her back in my arms.
Upon my return to the hospital the discussion of Discharge Plan came up. No Way!!!! Discharge Plan what’s that.
The lead NNP for Nia’s case, believed that it was critical to get Nia home so she didn’t contract any infections from being in the hospital too long especially in the medical team’s eyes Nia was one of the healthiest EVC babies they had cared for- WOW! Really? At Fairfax there seemed to be no end in sight- as it seemed the medical team only felt comfortable sending babies home on oxygen not actual respiratory support- like a ventilator. However, at duPont they were innovative in this department. They knew immediately how Nia could be fully supported at home in a safe environment.
There was even an ambitious discussion to have Nia home by Christmas, but we made the staff aware- there was no need to prematurely send Nia home- we need to make sure we had all our ducks in row.
In the meantime, Antoine drove in the wee hours of the morning to Wilmington after working long hours to FLEX his time so he could spend long weekends with us. I would eagerly await (using my time wisely- pumping overnight) at the Ronald McDonald House to let him in.
Learning Nia’s at home Care
We were shown what her home ventilator would like and how to properly use it. It was even “portable,” although heavy to carry. We were shown how to feed Nia via her g-tube and had to be proficient before discharged.
We took a CPR course at the hospital as well and watched numerous videos related to at-home care. While learning all of this we had to identify an in-home nursing company for Nia and coordinate meet and greets with the company we decided to go with. Additionally, we had to travel a few times back to our home in Alexandria to pick up Nia’s at-home equipment and meet with potential nurses that would care for Nia.
Nia’s Hospital grade home (portable) ventilator-respiratory support- Trilogy 
Meeting Another EVC baby and family in the hospital!
It was a blessing to meet another EVC baby (boy) and family! He took Nia’s old room- as Nia had gained a roommate in another room. It was a blessing to meet his family- Amish Dutch- in any other circumstance this would probably be unlikely meet between the both of us. Because EVC is so common in their community, we actually met their daughter who has EVC and some of their friends kids living with the condition. I was amazed! That gave us renewed hope that there is calm after the storm.
Breakfast with another EVC Family
We had another sweet family (non-Amish) that drove to meet me on a Saturday (Antoine had to work). There beautiful daughter has EVC, and she was absolutely adorable. She was strong and independent! I loved her spirit! So grateful again for social media- which led to this awesome met! 🙂
The Holidays at DuPont!
The holidays were actually not bad in the hospital considering our circumstances although we truly missed our family and friends. It was beyond exhausting though, living the hospital life, but we didn’t take this journey for granted. We had a baby to celebrate and be thankful for- what else could you ask for!
We learned more about Nia’s care.
We adjusted overall well to Nia sharing a room. Nia’s new NICU roommate was born prematurely on Nia’s due date, October 14! I don’t believe in coincidences- all part of God’s divine will! Baby Anya was so sweet and so was her family! It took a little adjustment sharing a room- but we managed well. For the first two months of our NICU journey, Nia had private single rooms.
Christmas Time
DuPont actually had a Christmas store for families to shop for free- it was so cool! We were able to get a couple of gifts for Nia, my nieces and nephews, And for ourselves- gift cards!
We were able to get a good home-cooked Christmas dinner with some family friends in Baltimore- and then back to Nia we went!
Nia’s First Christmas
 Nia at 3 months with her daddy! 😍
Nia at 3 months with her daddy! 😍

New Year’s Eve was Antoine’s bday so I had a day planned with the movies and dinner in Wilmington. Antoine loved the theater!
We brought in the New Year at Nia’s bedside.

End In Sight!
We were so close to going home by the beginning of January- and we were ready! We were completely exhausted from traveling back and forth to Wilmington- coordinating Nia’s in-home care and still trying to work at least somewhat- but we got it done!
Nia passed her car seat test with flying colors which is another required NICU benchmark! 🙌🏾😍
Nia’s car seat test! Someone was totally unbothered- 3 hours later! 💗💗💗

The Scramble to Finish Nursery
We couldn’t believe our baby would be coming home soon and the once blank guest room was now transforming into a nursery- Oh another miracle! To know we didn’t have a thing for Nia’s nursery prior to her birth, but somehow God provided- what a testament to God’s grace!
Nia’s nursery- fit for a NICU Warrior Princess!

Required Overnight In-Stay
Then it was time for our in-stay at hospital where you are required to do approximately 24 hours of care without any medical team help! That was an interesting night- because some things definitely remind you- this isn’t quite home but we survived!
Thennnn Graduation Day!
NICU graduation morning started off great, but then a glitch came that could’ve derailed Nia’s discharge… her g-tube Mic-Key had to be changed and we needed training on how to replace it if necessary- Say What!!!! We have checked the box for everything how was this miss???! I kept thinking noooo we have to get out of this hospital. We are done! Nia’s lead NNP was determine to rectify the problem and she did!

Doctors, nurses, and all other personnel came by to say their “see you laters.” It was an awesome feeling- Nia would get to finally see her nursery that we had only created after she was born!
Some of Nia’s awesome nurses/discharge team! 
As we walked out of Nia’s NICU room- I played “Pomp and Circumstance.” As I got to the NICU exit- I broke down in the most exhausting tears ever!!!! I said I wouldn’t cry but the joy and liberation that came over me was nothing but the Holy Spirit- Jesus kept us and Nia!

Walking out the hospital- 2nd NICU with a breathing and thriving baby was exhilarating and magical!!! It was truly another miracle!!! My God, My God! We survived! Walking out of the NICU with our baby in tow help to ease the heaviness of our journey.
We took our grand exit walk one last time and it felt so good!
In the car we went and 2 hours plus past Nia’s feeding time (she did soooo good) we finally arrived home to Alexandria, VA.
Nia’s at-home journey began…
“I can do all things through Jesus Christ that strengthens me.” Phil 4:13
“And We know that in all things God works for the good of those who love him, who have been called according to his purpose.” Rom 8:28
Journey Down NICU Memory Lane






































This blog post is dedicated to NICU Warrior parents! We pray our story enlightens family and friends of those on this journey that it’s truly a tumultuous journey that test your physical and mental capacity.
Be Blessed!
Erica
Team A&E


What a remarkable journey. I believe it’s no doubt that God chose you to be Nia’s parents because of your strong faith, dependency on him, strength, courage and willingness to do everything possible to help Nia grow and thrive. Thank you for sharing this amazing story. Your journal and these pictures have well told the miracle story of Nia’s first year. She is a strong little Lady whom I believe God will use in so many ways to help so many others. 💕🙏🏻👍💞
LikeLiked by 1 person
Thank you for sharing the beginning of Nia’s amazing journey! You are an awesome mother! Be blessed!
LikeLiked by 1 person
Thanks for sharing! Inspiring words of parents love and their trust in God. Continue to advocate for Nia’s care.
LikeLiked by 1 person
Amazing story, thank you for sharing. Reading your story and seeing the pictures from AI bring back memories for sure. My son was born July 20th 2018 and spend 47 days at AI, been home now for 4 months and loving it!! I am so glad that Nia is doing well and I pray for continued health for all of you guys!
LikeLiked by 1 person